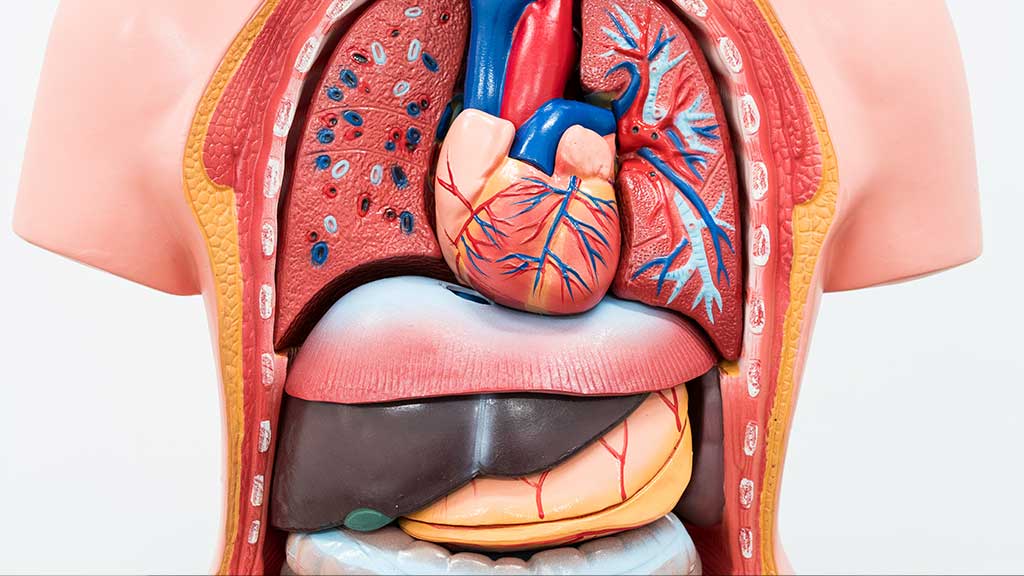
One of the most common complications of systematic inflammatory response syndrome (SIRS) is the onset of Multiple Organ Dysfunction Syndrome (MODS).
Although multifocal dysfunction syndrome does not follow a specific pattern, it usually begins with pulmonary insufficiency and continues with liver, intestinal, and renal failure.
Blood cell abnormalities and myocardial infarction usually appear late, but changes in the central nervous system can occur at any time.
Multiple organ dysfunction syndromes can also be caused by trauma to the tissue.
Acute respiratory distress syndrome, or diffuse intravascular coagulation syndrome, could be the components of MODS.
Although multiple organ dysfunction syndromes cause dysfunction in many organs, it also affects physiological systems that are not classically thought of as organ; including the circulatory system, immune system, or endocrine system.
Finally, although it is described as a syndrome, its course and clinical causes are highly variable.
Among the cases of primary multifocal dysfunction syndrome, the following can be mentioned
-
Pulmonary contusion
-
Acute kidney damage due to decreased blood supply
-
Coagulation disorders caused by multiple blood transfusion
Secondary multifocal dysfunction syndrome also occurs in the presence of inflammation or infection of distant organs from primary injury.
Patients with systematic inflammatory response syndrome and multifocal dysfunction syndrome are clinically hypermetabolic and have high cardiac output, low oxygen consumption, high venous oxygen saturation, and lactic acidosis.
Nutritional-medical treatment in multifocal dysfunction syndrome
Typically, critically ill patients are admitted to ICU intensive care units due to a diagnosis of the cardiopulmonary disorder, pre-and postoperative complications, multiple trauma, burns, or sepsis.
Hypoalbuminemia is a reflection of the disease and the severity of the injury and inflammation; therefore, serum albumin should not be used as an indicator of nutritional status. Other plasma proteins, such as pre-albumin and transferrin, are often severely depleted, not due to nutritional status, but due to a decrease in inflammation-induced hepatic synthesis and changes following fluid displacement. The body is to another part.
This is part of the acute phase response in which secreted and circulating proteins are modulated in response to inflammation or damage.
Food or fluids may be severely restricted because the patient is very ill.
Here are some common nutritional-related issues
-
Insufficient food and drink intake (other methods of prescribing food and fluids are needed).
-
Inadequate or excessive food intake through enteral (EN) and parental infusions
-
Inadequate or excessive fluid intake (due to intravascular infusions, nutrient solutions, or fluid excretion through the feeding tube)
-
Increased nutritional needs (such as protein for wound healing)
-
Excess carbohydrate intake (for example, when a parental solution is given to a patient with chronic malnutrition and possibly prone to malnutrition syndrome).
-
Abnormality of nutrition-related laboratory results
-
Altered gastrointestinal function (such as vomiting, diarrhea, and constipation)