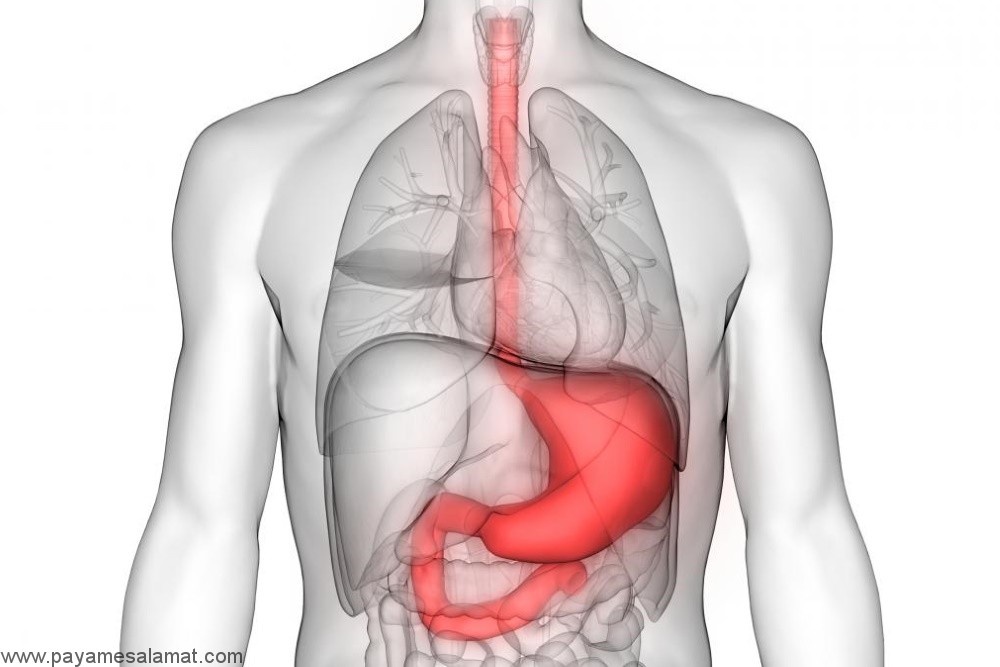
Gastritis is a non-specific word that literally means the inflammation of the lining of the stomach. The term is used to describe gastric-associated symptoms, an endoscopic manifestation of the gastric mucosa, or a histological change with epithelial infiltration by inflammatory cells such as multinucleated PMN cells.
Types of gastritis
-
Acute gastritis: Acute gastritis refers to the sudden onset of the inflammatory process and the symptoms.
-
Chronic gastritis: Chronic gastritis occurs over several months to decades with the recurrence of signs and symptoms. Prolonged gastritis may lead to atrophy and loss of gastric wall cells that reduce acid output and internal factor secretion. These alterations can finally result in pernicious anemia.
-
Obstructive gastritis: Another type of gastritis is obstructive or erosive gastritis that is less common than acute and chronic type. Although, the obstructive gastritis is not a severe ty, it can result in bleeding and severe stomach ulcers.
Causes of gastritis
-
Consumption of alcoholic drinks or long-term use of nonsteroidal anti-inflammatory drugs such as ibuprofen.
-
Extensive surgeries
-
Severe burns
-
Severe trauma and infection
Symptoms of gastritis
Signs and symptoms of gastritis include:
-
Burning pain (indigestion) in the upper abdomen that may get better or worse with eating.
-
Nausea
-
Vomit
-
Feeling of fullness in the upper abdomen particularly after eating (feeling heavy)
-
Flatulence or abdominal bloating
Diagnosis of gastritis
Gastritis can be diagnosed based on clinical signs and symptoms and medical history (e.g., NSAID or alcohol consumption) or laboratory tests (e.g., breath, blood, stool, immunological, and biopsy tests to detect H. pylori) and other tests (such as endoscopy or radiological tests).
Non-invasive methods for diagnosing H. pylori include a blood test for H. pylori antibodies, the urease breath test or the stool antigen test.
Peptic ulcers
The digestive tract cells are protected against the stomach acid and pepsin (an enzyme that breaks down proteins) from being auto digested, with some defensive mechanisms e.g. secreting mucus or bicarbonate ions to neutralize acid, washing away the permeating acid with mucosal blood flow, rapid regeneration of damaged epithelial cells, etc. Peptic ulcers are open sores in the inner lining of the stomach or the upper portion of small intestine, that occur as a result of the failure of the defense and repair mechanisms. For a symptomatic peptic ulcer, more than one of these mechanisms must be impaired.
Peptic ulcers usually show evidence of chronic inflammation and repair stages around the lesion.
Causes of peptic ulcers
-
H.pylori infection
-
Gastritis
-
Taking aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids
-
Severe diseases
Nutrition and medical treatment regimen in gastritis
Treatment for gastritis involves the removal of stimulants (for example, pathogens), nonsteroidal anti-inflammatory drugs, or NSAIDs. Antibiotics and proton pump inhibitors (PPIs) are basic medical treatments. The side effects of suppressing gastric acid secretion, both due to disease and due to proton pump inhibitors, should be considered.
These side effects include decreased gastric acid output which can reduce the absorption of nutrients (such as B vitamins, vitamin C, calcium, etc.) since gastric acid is required for intragastric proteolysis and food digestion.
Suppressing gastric acid secretion may increase the incidence of bone fractures as well as the risk of recurrent infections because gastric acidity is a primary defense factor against ingested pathogens.
The symptoms of gastritis can be aggravated by chemical stimulants. To treat gastritis, all of the stimulants must be reduced or stopped. For example: stop smoking, avoid excessive alcohol consumption, avoid caffeinated and carbonated beverages, and drink juices that contain citric acid (e.g., grapefruit, oranges, pineapples, etc.), and Avoid high-fat foods.
There is no gastritis diet; However, H. pylori may grow with a high-fiber diet or foods that contain flavonoids (e.g., tea, onions, garlic, berries, celery, cabbage, broccoli, parsley, thyme, soy and legumes).
What items in the diet make the symptoms of gastritis worse?
Foods that are high in fat may make inflammation of the stomach worse. Some other foods that irritate the stomach include:
-
Alcohol
-
Coffee: Coffee is acidic in nature and its consumption can intensify the feeling of heartburn.
-
Acidic foods such as tomatoes and some fruits
-
Acidic fruits and juices: Acidic fruits including oranges, sweet lemons, sour lemons, grapefruit
-
Fatty foods
-
Fried foods
-
Carbonated drinks
-
Spicy foods
-
Allergenic foods that cause inflammation: processed foods such as white bread, pasta, products containing excess sugar, trans acids, refined oils, fried foods